Bioresorbable synthetic polymers were first introduced as medical devices in the late 1960s for sutures made of glycolic and lactic acid-based polymers. They continue to have broad applications in orthopaedic devices and as a component in bioresorbable biocomposites, drug delivery, cardiovascular applications and regenerative medicine. Further, current research and investments indicate a future where new bioresorbables will replace the current materials in orthopaedics.
The basis for developing bioresorbable devices was to eliminate the need for re-operation (e.g. sutures, bone screws and plates), eliminate stress shielding and enable normal regeneration of tissue, improve imaging capability and improve ease of revision.1,2 The early research of bioresorbable polymers led to the definitions of bioresorption in the context of degradation of polymers in vivo, and importantly, the degradation of products being safely metabolized and resorbed within the body while not eliciting an adverse reaction, and causing minimum consequences to the patient.
David F. Williams, Ph.D., Professor at the Institute for Regenerative Medicine at Wake Forest University, is considered one of the world’s leading authorities on biomaterials. Professor Williams has defined bioresorption as “the process of removal by cellular activity and/or dissolution of a material in a biological system.” The foremost performance requirement is biocompatibility, defined as “the ability of a biomaterial to perform its desired function with respect to a medical therapy, without eliciting any undesirable local or systemic effects in the recipient or beneficiary of that therapy, but generating the most appropriate beneficial cellular or tissue response in that specific situation, and optimizing the clinically relevant performance of that therapy.” The criteria for the ideal bioresorbable polymer is defined as: “does not evoke an inflammatory/toxic response, disproportionate to its beneficial effect; is metabolized in the body after fulfilling its purpose leaving no trace; is easily processed into the final product form; has acceptable shelf life; and is easily sterilized.”2
The balance of this article is focused on the transition away from Poly-L-lactic acid (PLLA)-type resorbable polymers to updated and novel resorbable biomaterials that are designed to perform better clinically.
Historically Dominated by PLLA Class Resorbables
PLLA is a semi-crystalline polymer that was first researched for resorbable sutures in the late 1960s and into the early 1970s, and used in the 1980s and 1990s for fracture fixation devices. The underlying concepts include being sufficient in strength for load bearing and repair of tissues or bones, followed by gradual resorption and transfer of stress to newly-forming tissue (regeneration) and complete resorption of the suture or device, obviating the need for removal.1,2,3
The crystalline regions of both Polylactic acid (PLA) and PLLA hydrolyze much more slowly than the amorphous regions, and chain-end scission is negligible to non-existent for neutral and basic pH solutions, with enzymatic interaction known to further biodegradation.4 It is this mechanism of degradation, combined with the chemistry, size and shape of degraded solid polymer, that is now known to contribute to low-level, persistent, long-term chronic inflammation and lack of bone formation replacing PLLA.
In the early- to mid-1990s, PLLA and Poly-DL-lactic acid (PDLA) resorbable polymer devices were developed for fracture repair in pediatric maxillofacial and craniofacial applications. Within this same timeframe and into the early- to mid-2000s, PLLA and PLDLA and other similar materials and blends were developed for ligament and tendon fixation to bone, and for suture anchors. As clinical use proliferated, so did reports of complications and adverse findings of the devices. In 2007, the negative aspects of PLLA-based devices were reported: “Though biocompatible, the excessive longevity of PLLA (>3 years) and the absence of its replacement by bone indicates that despite being satisfactory clinically, it is not an ideal implant material, and that improved absorbable materials need to be developed.”5 More recently in 2016, a comprehensive article was published about biocompatibility, foreign-body reaction, cellular interaction, implant degradation, histopathology and adverse effects of PLLA devices leading to undesirable clinical side effects.6
Between the mid-2000s to mid-2010s, PLLA-based meshes and 3D-braided scaffolds received FDA 510(k) clearance for augmenting soft tissue repair (Synthasome, Inc.; Soft Tissue Regeneration, Inc.), and a ligament-device for ACL reconstruction (PMA) was trialed by Soft Tissue Regeneration, Inc. in a 15-patient pilot study in the Netherlands. Subsequently, the company has since rebranded as Biorez and has not yet published clinical data. Biorez representatives advised that 36-month human data will be presented at AAOS in March 2019.
Starting in the mid- to late-2000s, the need for improved resorbable biomaterials for fixation devices, scaffolds and meshes for soft tissue repair and augmentation were clearly established, which led to the decline and elimination of PLLA-only devices existing in today’s marketplace.
Transitioning to Better Formulated and New Resorbbale Polymers/Biocomposites
Surgeon and clinical drivers for better tendon and ligament fixation include:
- Simplicity, speed and ease of surgery with similar or better strength of fixation;
- Minimal creep or slip of the ligament, tendon or suture-anchored reconstruction;
- Better biological resorption profile; and
- Higher strength to eliminate potential failure on insertion.
Likewise for meshes and scaffolds for primary reconstruction and augmentation of injured or severed soft tissue structures, clinical and surgeon drivers include:
- Strength of device maintained through healing and start of maturation period;
- Biocompatibility and minimal to no adverse biological reaction;
- Ease of use in arthroscopic procedures, and;
- Reliable clinical outcomes similar or better than autograft.
For tendon and ligament fixation with resorbable materials, ACL reconstruction with interference screws dominates the number of procedures, and rotator cuff repair dominates the clinical application of suture anchors. The large companies offer several common non-resorable and resorbable materials for fixation devices, with PLLA-only use almost non-existent, and biocomposites and PEEK increasing in use.
A primary driver for developing biocomposites was substitution of a significant percent of the “offending” resorbable polymer with well-known, biocompatible and bone-friendly calcium phosphate (CaP) based materials such as beta-TCP, CaS, sintered and unsintered HA and blends of two or more CaP materials. The development of biomaterials to improve long-term tissue compatibility with devices has seen the substitution of some of the PLLA with faster resorbing, more biologically-friendly materials such as polyglycolic acid (PGA), caprolactone and polethylene glycol (PEG), and also modulate resorption rate relative to the base PLLA and/or PDLA material.
In other words, today’s biocomposites are more biocompatible and likely replaced by bone because of the substantial percentage of CaP material (25% to 60% by weight), elimination of PLLA and substitution of more biologically-friendly polymers.
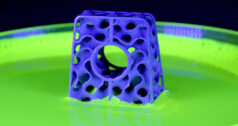
There are several resorbable synthetic materials for meshes and scaffolds based on weaving or knitting of fiber-based materials for repair and augmentation of soft tissues (excluding sutures), with one notable material being Poly-4-hydroxybutyrate (P4HB, Tepha, Inc.), which has been described as a new generation of resorbable biomaterial for tissue repair and regeneration devices.7 P4HB is a thermoplastic, linear polyester, produced by recombinant fermentation, with fibers that are extruded into strong, elastomeric material with strength retention ideal for soft tissue repair and augmentation.
What Does the Future Hold?
Progress in orthopaedic biomaterials and devices has occurred incrementally and deliberately over the past 50 years, owed in part to surgeons’ and corporations’ justifiable risk aversion, the regulatory process and an increasing demand for evidence before moving to the “next thing.”
Recent new resorbable materials such as Smith & Nephew’s REGENESORB show that improved formulations of historical polymers (PLLA+PGA=PLGA) and CaP materials (beta TCP and CaS) can produce higher-strength, biocompatible fixation devices that are more aligned with clinical and surgeon demands.
It is also certain that new classes of resorbable biomaterials will be developed, as exemplified by Acuitive Technologies’ CITREGEN™, which in one formulation is 60% HA and 40% poly(octamethylene citrate) polymer. CITREGEN’s polymer is characterized by a citrate-based network of cross-linked amorphous polymer chains, which subsequently results in uniform hydrolysis kinetics without the bulk degradation or acid dumping reported for PLLAs.8
Expect investments by both startups and large companies to continue in order deliver improved and novel resorbable biomaterials that will meet clinical and surgeon demands. These resorbables will slowly supplant permanent materials such as PEEK, titanium and the biocomposites of the present.
References
[1] Williams, David, The Biocompatibility, Biological Safety and Clinical Applications of PURASORB® Resorbable Polymers, An Independent Report Compiled for Purac Biomaterials, Editor-in-Chief, Biomaterials, Partner, Morgan & Masterson LLC, May 2010.
[2] Middleton, JC, Tipton, AJ, “Synthetic Biodegradable Polymers as Orthopedic Devices”, Biomaterials 21 (2000), pp 2335-2346.
[3] Barber, F. A., Dockery, W. D. (2006). Long-term absorption of poly-L-lactic Acid interference screws. Arthroscopy, 22(8), 820–826. doi:10.1016/j.arthro.2006.04.096.
[4] Henton, David, Gruber, Patrick, Lunt, Jim, and Randall, Jed, “Chapter 16 – Polylactic Acid Technology”, in Nano Fibers, Biopolymers, and Biocomposites, pages 528 – 568; 2005, CRC Press
[5] Walton and Cotton, J of Biomaterials Applications, 2007 21:395.
[6] Y. Ramot et al., Advanced Drug Delivery Reviews, April 4, 2016, 107:153-162
[7] Simon F. Williams, Said Rizk and David P. Martin, Poly-4-hydroxybutyrate (P4HB): a new generation of resorbable medical devices for tissue repair and regeneration, Biomed Tech 2013; 58(5): 439–452
[8] For the references to Acuitive Technologies Citregen Biomaterial: (Hu et al., PNAS, 2010 and Davies et al., PNAS, 2014).
Robert A. Poggie, Ph.D., is President of BioVera. His previous employers and functions include Smith & Nephew, Implex, Zimmer and Pipeline Orthopaedics, with responsibilities in applied research, biomaterials, clinical research, medical education and regulatory affairs. He can be reached by email.