The trend in newly-launched spinal cages has been a focus on expandables and additively manufactured devices, with a shift away from traditional manufacturing with all-PEEK to those that incorporate titanium, whether in the coating or the body.
Neither manufacturers nor surgeons have reached a consensus on whether or not spinal cages should be 100% PEEK, coated PEEK or titanium. What can’t be disagreed on is the fact the shift away from all-PEEK cages is a direct response by device companies, based on what they’ve been hearing from surgeons, to manufacture implants using materials or coatings with greater strength, porosity and bone-ingrowth capabilities.
With this in mind, and in an effort to get a better understanding of what is happening in this space, we posed questions on spine cage technology to three veteran spine surgeons.
While all three confirmed the shift to incorporate titanium, they also provided insight which we thought you would find interesting—including a forecast for the next five years in cage technology and thoughts on device companies’ priorities.
Michael Steinmetz, M.D., is Chairman of the Department of Neurosurgery at the Cleveland Clinic Neurological Institute.
He also serves as the vice president of the Congress of Neurological Surgeons, secretary of the Council of State Neurological Societies, an executive committee member of the AANS/CNS Section on Disorders of the Spine and Peripheral Nerves and is involved with the American Association of Neurological Surgeons, the North American Spine Society and the Society for Neurosciences.
What are your thoughts on cages that are expandable, additively manufactured or those that incorporate titanium?
Dr. Steinmetz: Cage design has been a game changer in spine surgery. Surgical approaches have been somewhat stagnant, but cage design has made surgery easier and potentially safer. Cages require an appropriate “fit” in the interbody space to effectively fuse. If too loose, fusion may not occur; if too large, endplates may fracture or be “plowed” during insertion, resulting in subsidence and construct failure. More importantly, cage placement in the posterior transforaminal route places both the traversing and existing nerve roots at risk of damage during insertion. This may result in the surgeon choosing too small of a cage to lessen the chance of nerve injury, but increase the risk of unsuccessful fusion.
Expandable cage design permits a smaller cage to be inserted in the disc space, hence easing the chance of nerve and endplate injury, but after expansion an appropriate fit to the endplates.
What are the benefits to these cages?
Dr. Steinmetz: Material properties have increased fusion rates, at least anecdotally. Cages made of PEEK were advantageous, as the modulus of elasticity is similar to bone and are minimally visualized on x-ray and CT. The cage may have a decreased chance of subsidence due to its modulus, and fusion may be more easily visualized due to its radiolucency on imaging. But these cages are limited, as they do not integrate with bone. Specifically, bone does not grow into the cage, which may be problematic.
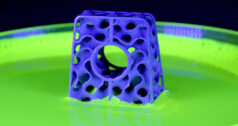
Additively-manufactured cages made of titanium or alloys are designed to match the porosity of normal bone. The metal properties and porosity have shown increased bone attraction and ingrowth into the cage. I have seen an increase in successful fusion with these newer designs. These could perhaps be considered biologic cages, as opposed to simple cages.
Are there other technology advancements that you think device companies should be prioritizing?
Dr. Steinmetz: Currently, the two most significant advances are robotic and metal properties, including 3D printing. I think most companies are currently prioritizing these two areas. Robotics merging with computer assisted navigation will likely change how we perform spine surgery five to 10 years from now.
Robert S. Bray Jr., M.D., founded DISC Sports & Spine Center in 2006.
Dr. Bray launched DISC after tenure at Cedars-Sinai, where he had founded The Institute for Spinal Disorders. He has also served as the director of neurosurgery and headed the spinal programs at St. John’s Medical Center, Century City Hospital and Daniel Freeman Memorial Hospital.
What are your thoughts on expandable cages?
Dr. Bray: The concept of an expandable cage is a very valid and useful one, when you consider minimally invasive procedures. Currently, I don’t use expandable cages because I think they’ve failed. I think the device companies are sort of missing the point in some of the design aspects. I think the technologies will grow, but they are on a slow learning curve.
In general, what are device companies missing with their cage technologies?
Dr. Bray: The biggest thing with any implant, including intervertebral, is first, do they work? Not how cute the technology is. In the long run, does it work for the patient? One, the surface of the implant has to bind with the bone. Two, the area of the fusion that ultimately happens for the patient or the amount of surface it fuses has to exceed the surface of the implant. In the design, a number of products have failed in implementation as the device companies have failed to apply these principles.
My experience, and that of many others, is that PEEK routinely gets a poor binding to the surface of the bone and often causes an inflammatory reaction around the implant.
What will the spine industry be saying about cages five years from now?
Dr. Bray: Versions of implants will exist that have better surface areas and better binding. I see a reduction in PEEK, if not being replaced altogether. I see devices getting simpler and certainly not more expensive. Making implants more complex and more expensive doesn’t really answer what’s going on in medicine. I’m sensitive about something that costs $1,000 or $2,000 more because it has a cute little ratchet in it.The basics of bone binding to whatever the surface may be, whether it’s coated or just titanium, I think that’s very important.
Design is going to remain very important and the basis of forming fusion and the weight-bearing characteristics of the implant will remain important principles.
What else do you see happening in spinal cages?
Dr. Bray: I applaud people for looking at new designs and new possibilities. For routine degenerative spine, I think technology has to keep changing and evolving. There are some good concepts, but I don’t think they’re there. Companies have to return to the basics and ask themselves why they’re doing this—and not just for marketing purposes. Are you getting positive outcomes for the patient? Are you increasing cost efficiency? Is the implant of quality? Are you decreasing complication rates? If you are doing all of that, you’re moving the mark forward. Implant companies have to be on board with where medicine is going.
Stephen H. Hochschuler, M.D., is a Co-Founder of the Texas Back Institute.
He has over 30 years of experience and specializes in lumbar problems. He is President and a founding member of the Spine Arthroplasty Society, past Chairman and current Board of Director at SpineMark and Founder of the Spine Division at the Veterans Administration.
What is shaping the spinal cage market right now?
Dr. Hochschuler: In my world, the patient is always in the center, but part of that is safety, efficacy, etc. Most good surgeons have no problem putting in any cage. The new cage technology has its benefits: faster healing, covering more surface area and ease of implant. Especially now, as everyone is focusing on minimally invasive procedures.
Are you using cages that are expandable, additively manufactured or those that incorporate titanium?
Dr. Hochschuler: I have used them, but I stopped operating one year ago, after 40 years of surgery. That said, we have over 20 spine surgeons at the Texas Back Institute and they use them.
When it comes to expandables, the only one that can expand mediolaterally and height-wise, that I know of, is made by Integrity Implants. They have a cage that’s unreal.
What will the next five years bring in spinal cage technology?
Dr. Hochschuler: Device companies need to focus [their products] on simpler, faster minimally invasive procedures that can be done in ASCs. With 3D printing, you’re going to get more in terms of individualized medicine. You’ll probably be able to match exactly what you want to do, per level, per patient and I envision every hospital will have its own 3D printer. The manufacture, distribution and utilization are all going to change. Titanium has been fine and new titanium is even better. I think memory alloy could be important.
How about a minimally invasive approach where you build a cage inside the disc space? That’s a futuristic thought. How will you do that? Right now, I don’t know. But can you do that? Absolutely. It’s a matter of exploring the technology, what it would cost, etc. What I love about spine is that it’s always changing. It’s interesting to watch how the approaches change.
Rob Meyer is ORTHOWORLD’s Senior Editor. Please send comments on this article to Carolyn LaWell.