Post-surgical infection control remains a topic of importance in orthopaedic product development, as surgeons, researchers and device companies continually seek to reduce complications, readmissions, revisions and cost. The sense of priority was validated at OMTEC® 2017, when these groups met to address infection prevention—and the discussions carried throughout the entire conference.
The number of infected total hip and total knee replacement procedures combined is expected to reach 70,000 in 2020 according to Matthew Dietz, M.D., OMTEC speaker and an orthopaedic surgeon at West Virginia University School of Medicine. That infection burden alone is expected to cost $1.6 billion.
Dr. Dietz challenged device companies to create not only implants that prevent infections, but also technologies that assist in rapidly diagnosing and testing for infections.
In recent months, our own conversations with industry around infection prevention have related to combining ionic silver and antibiotics with materials.
As your R&D team considers infection prevention, we share with you this BONEZONE article from July 2016, which reviews how competitors in the trauma space are tackling the issue.
New Trauma Technologies Emerge to Treat Infections
BONEZONE, July 2016
By Hannah Corcoran
In the trauma market, the third-largest segment in the orthopaedic industry, technologies intended to minimize post-surgical infections are emerging as a potential solution to address rising healthcare costs.
Infection control has been on the radar of various orthopaedic device companies, from startup to top five. Earlier this year, Stryker announced its $2.7 billion acquisition of Sage, a developer and manufacturer of disposable products targeted to reduce “Never Events” such as infections. In 2015, DePuy Synthes mentioned infection control as a priority, though they offered little detail.
Though post-surgical infections can occur in any segment in orthopaedics, trauma procedures may be more prone to infections due to the unexpected and urgent nature of those cases.
Several OEMs have introduced technologies to address infection control using various materials and techniques, such as antibiotic coatings, surface modification, combination devices, disposables and sterile instruments. Here, we examine how these approaches work.
Approach #1) Tri-Calcium Phosphate Bone Void Filler
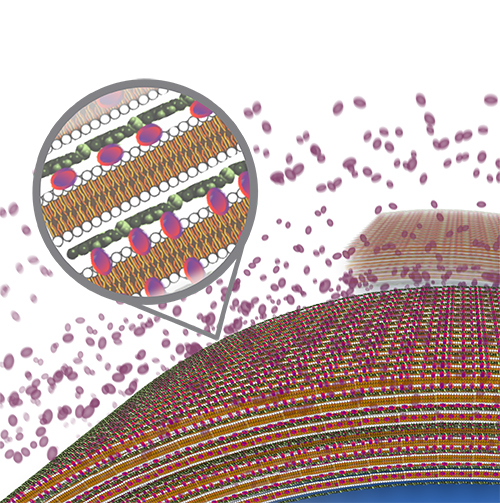
PolyPid is conducting a clinical trial of BonyPid-1000™, described by the company as a drug/device combination containing tri-calcium phosphate bone void filler and the company’s PLEX platform technology. The PLEX encapsulation matrix contains an antibiotic that is released locally over 30 days, says Dikla Czaczkes Akselbrad, PolyPid’s Chief Strategy Officer.
The BonyPid approach combines four attributes: local administration, a broad spectrum antibiotic, pre-determined and prolonged periods of release and a small, safe overall dose that generates high local concentration.
Local administration plays a particularly important role in this approach, Czaczkes Akselbrad says.
“The standard of care includes systemic administration [of antibiotics into the bone void], which is limited due to low penetration into the needed site. Local delivery may overcome this issue. However, the approved local solutions are characterized by short-term and non-controlled release of the entrapped drug,” she says.
“Currently, in the U.S., the only approved local delivery is based on a cement polymer that releases an effective amount of antibiotics over a short period (several days), which is also characterized by high burst release. This release profile is limited in the eradication of significant bacterial load, and can even lead to resistant strains of bacteria.”SP
BonyPid-1000 is undergoing a pivotal clinical study for CE Mark approval, and PolyPid plans to submit an IDE by the end of 2016 for further FDA approval.
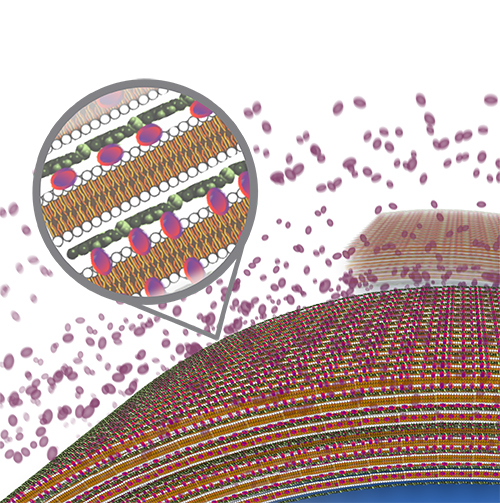
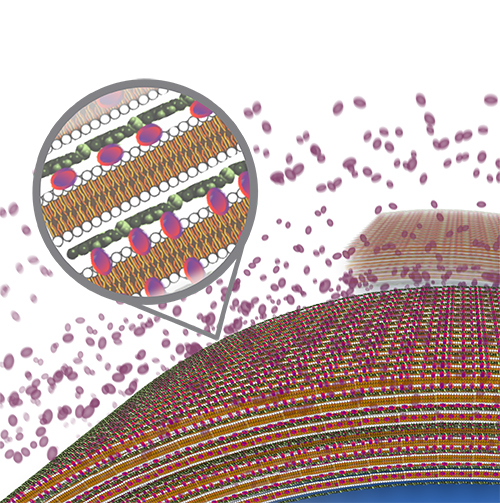
Graphic rendering of PolyPid’s BonyPid-1000
Approach #2) Antimicrobial Silver Ion-Eluting Bone Screw
Silver Bullet Therapeutics’ approach to preventing infections in trauma is the OrthoFuzIon Antimicrobial Bone Screw, which uses an electrical charge to release a cloud of antimicrobial silver ions around the implanted device. The product received its CE Mark in March 2015, and FDA approval is expected in 2016.
The system is powered by a self-sustaining battery that co-sputters silver with platinum to release silver ions into the local area around the implant, creating that cloud of anti-infectivity, according to Paul Chirico, Co-Founder, President and CEO of Silver Bullet Therapeutics.
“The wonderful thing about silver is that it’s localized, so it stays where you need it,” he says. “That’s also the bad thing about silver. It’s not a systemic, unlike some companies that have gone in the direction of antibiotics, which are systemic and have tremendous hypersensitivities associated with them.”
Chirico noted that the company developed bone screws to prevent infections first, because trauma is the “toughest area in orthopaedics” to mitigate post-surgical infections.
Approach #3) Modifying Surfaces with Nanotechnology
Tyber Medical worked with Thomas Webster, Ph.D., Chair and Professor of Chemical Engineering at Northeastern University, to develop its process to prevent infections. Tyber Medical is using nanotechnology with its BioTy™ Modified Surface Treatment, which can be applied to titanium, stainless steel, cobalt chrome and PEEK. The surface modification process creates a texture designed to be a bacteriostatic surface to reduce the adhesion of bacteria and biofilm formation.
Tyber Medical has received two FDA 510(k) clearances for BioTy on the company’s headed, headless and snap-off screw systems. The systems are available to the company’s private label partners and are indicated for use in the extremities for bone fixation, bone reconstruction, osteotomies, arthrodesis, joint fusion and fracture repair.
Webster has studied the use of ceramic nanomaterials to control surface energy to decrease infection, promote bone growth and inhibit inflammation.
“Nanotechnology allows you to increase the surface area of your implant. So if you took a ceramic implant and made it out of nanomaterials, you’d have much more surface energy,” he says. “That allows you to control the charge of your surface, which also allows you to increase the absorption of things like LubriSyn, so you can keep that ceramic from becoming infected.”
Conclusion
Not surprisingly, each company employing or developing these new technologies has arguments for their approach and against others.
Silver Bullet Therapeutics’ leadership, for example, is skeptical that coatings can prevent infections in trauma.
“You could take an antibiotic and paint it on, which sounds like a great idea, but it really isn’t,” says Bohdan Chopko, M.D., Ph.D., Co-Founder of Silver Bullet Therapeutics and Associate Professor of Neurosurgery for Stanford University. “The antibiotic-coated device idea has a lot of issues, from patient sensitivity to antibiotics, to controlling the release, to having it scrape off if you’re placing a screw into bone.”
Further, there are distinct issues with technologies that elute a pharmacological drug or a metal ion, versus technologies that modify surfaces, says Rui Ferreira, Vice President of Research & Development at Tyber Medical.
“The challenge is that either one of those will work for a time, but a dose response dilution will be associated,” he says. “It’s going to start off having an effect, but will change over time because as it elutes, it leaches off and that causes challenges from FDA.”
Webster and Ferreira agree that antibiotics aren’t cutting it and may be breeding resistant strains of infections.
“The challenge with orthopaedic implants is that once bacteria colonizes on implants and forms biofilms, regular pharmaceutical treatments can’t eradicate the infection; you can’t get it killed and cleaned off of the implant,” Ferreira says.
The widespread production, use and misuse of antibiotics have contributed to the next generation of drug resistant infectious organisms, commonly called superbugs.
“The problem is that we thought antibiotics would be the solution, so that was really the only approach. We know now that doesn’t work,” Webster says. He added that new chemistries are emerging to kill bacteria and increase bone growth, such as selenium, though they would likely take over a decade for FDA to approve.
Despite this activity, it is too early to determine whether these types of devices will prevent infections. Research conducted outside of trauma, such as the use of sensors in joint replacement stems, may offer a future solution. Further, the issue of whether or not hospitals and surgery centers will actually pay for new technologies and cutting-edge devices will ultimately depend on long-term outcomes to demonstrate cost savings. Companies commercializing these technologies argue that if a certain patient population is prone to infection, a higher price might be justified if the technology can prevent infection.
Send comments on this article to Carolyn LaWell.




