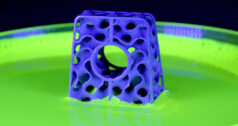
Scientists have programmed stem cells to grow cartilage on a 3D woven scaffold shaped like a femoral head, results that could lead to an alternative to hip replacement for arthritis patients.
The technique, which was described in the Proceedings of the National Academy of Sciences, takes mesenchymal stem cells from fat and seeds them on a biomaterial scaffold that can then be implanted onto the surface of a hip. Further, the scientists added gene therapy to cells to release anti-inflammatory molecules that not only resolved damaged cartilage, but staved off arthritis.
“This is the first time we’ve seen anything where we’ve been able to make functional cartilage with the properties of cartilage that’s virtually unlimited in size,” says Farshid Guilak, Ph.D., a professor of orthopaedic surgery at Washington University. “You can make it the size and shape of an entire joint.”
The research is being conducted between Washington University School of Medicine in St. Louis and Cytex Theraupeutics in Durham, North Carolina. Guilak also serves as President of Cytex and formed the company with colleagues before he moved from Duke University to Washington University.
“Nearly all of the approaches that are being used now for cartilage repair focus on studying what we would call a focal defect,” Guilak says. “It’s like if you had a pothole in the road, if you have a chunk of cartilage missing; virtually every approach is designed now chemically to fill that pothole. As our lab worked on osteoarthritis, what we saw was there is really no treatment for whole joint degeneration in this manner. The only thing you can do is diet and exercise, take Motrin and then have a joint replacement. There are no treatments that affect the course of the disease. So we started to work on this concept of, can we regenerate cartilage, not just to fill a little hole, but to repave the entire road? To do that, you need a lot of cells and you need a biomaterial scaffold that can form in the shape of a hip or a joint and can withstand loading that can be several times your body weight through your joints.”
The group’s research is focused on the hip, specifically arthritic hips in patients 40 to 60 years of age. By regrowing and replacing the cartilage, they believe they can provide a solution that extends the longevity of the joint and delays—or even eliminates—the need for a total replacement.
The current research is focused on resurfacing the femoral head, Guilak says. The hope, though, is that eventually the technique will be applied to full resurfacing of both sides of the joint and then repeated for success in other joints, like knee and shoulder.
Large animal studies are underway. The expectation is that they’ll move to clinical studies in humans in the next three to five years, says Bradley Estes, Ph.D., Vice President of Research and Development at Cytex.
Study of the anti-inflammatory or gene therapy combinations will have a longer regulatory process through FDA. Guilak describes the approach as such:
“The gene that we used was for the inhibitor of a very potent inflammatory molecule called Interleukin-1, and it’s involved in osteoarthritis and rheumatoid arthritis. It starts a lot of the inflammatory cascades. We put in a gene that inhibits Interleukin-1 called IO 1 receptor antagonist. It’s a drug that’s sold now as Kineret or Anakinra; it’s approved for rheumatoid arthritis, but it’s a naturally occurring molecule. It’s a biologic molecule, so if you put the gene into the cell, it will produce that molecule. The other thing we did is put a part of the gene in so that we can turn the IO 1 receptor antagonist on and off, so it’s not spewing out all the time in the joint. We can control, in what we call a tunable and inducible manner, how much is being produced. If we give the cells a small activating molecule, we just use doxycycline as an activator of this gene, and we can actually turn on the anti-inflammatory delivery, or we can turn it off by removing doxycycline.”
Cytex’s largest barrier to commercialization, as for many small companies, is funding, says Estes. The team has spent nearly 15 years researching this technology and thus far the funding has been there.
The research has been funded mainly through grants from entities like National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institute on Aging of the National Institutes of Health, AO Foundation, Arthritis Foundation and the National Science Foundation. — Carolyn LaWell
CL
Carolyn LaWell is ORTHOWORLD's Chief Content Officer. She joined ORTHOWORLD in 2012 to oversee its editorial and industry education. She previously served in editor roles at B2B magazines and newspapers.