Researchers at The University of New South Wales (UNSW) in Sydney, Australia have developed a fusion device designed to stabilize the spine without use of bone graft or pedicle screws for single-level posterolateral fusion. After years of development and preclinical testing, the first clinical trial will begin before year end. Update, October 2016: Per Dr. Walsh, human clincial trials will commence in 2017, rather than the previous expectation of 2016.
The inventors assert that the Thru-Fuze™ device can simplify spinal fusion, and make procedures faster and less expensive than existing methods.
Thru-Fuze differs from traditional posterolateral fusion, which requires autograft harvesting or bone graft materials and pedicle screws to be placed into the spine to provide mechanical stability and participate in the fusion, says co-inventor William Walsh, Ph.D., Professor and Director of the Surgical & Orthopaedic Research Laboratories at the Prince of Wales Clinical School at UNSW.
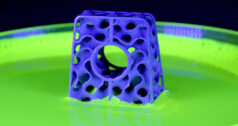
Walsh and co-inventor, Matt Pelletier, Ph.D., suggest that, rather than having to grow bone from one particle of bone graft to the next to achieve fusion, bone could grow through small holes in the device and form a bridge between the vertebrae. (Pelletier is a Lecturer and Research Fellow at the Surgical & Orthopaedic Research Laboratories at UNSW.)
“When you do a posterolateral fusion with pedicle screws, you shift the mechanics posteriorly (to the rear). The Thru-Fuze is in the middle, so the strains are more physiological, causing bone to grow across the device,” Walsh says.
At the time of implantation, the device provides rigidity in axial rotation and lateral bending, but the spinal segment remains slightly compliant in flexion-extension. As the body integrates into the device, the spine is stabilized, according to Walsh. The bone formation into the device provides the “glue” for integration and stability.
Walsh compares the way that the device works with the body’s natural healing response, similar to when you hit your shin and get a bump on your tibia. “That’s all you need to do to integrate into the device. You just need that initial pulse of bone healing after the surgeon prepares the host bone,” he says.
Omitting autograft makes the surgery less traumatic, because it minimizes blood loss and potential complications. Omitting bone graft substitutes and pedicle screws also reduces operative time, because the approach doesn’t rely on complex instrumentation and preparation, Walsh says.
Thru-Fuze is intended to reduce costs, because you don’t have to purchase synthetic bone graft for the procedure or use imaging, since you’re not going through the pedicle.


- An illustration of the Thru-Fuze concept in action.
Researchers conducted a pilot study to test their hypotheses. Following its successful completion, Xinova invested $2.3 million in the research, design and development of Thru-Fuze. Walsh and Pelletier worked with Orchid Orthopedic Solutions to develop the concept; Orchid created the Design History File and Device Master Record, and then machined Thru-Fuze from titanium Grade 5 alloy with a porous interconnecting coating on the interior.
Prototypes were also made in Walsh’s lab through 3D printing to test geometry, supporting convenient creation of iterations.
After the device was manufactured, researchers tested performance in large animal studies. Thru-Fuze was implanted in adult sheep. Fusion was achieved at six weeks and new bone formed under and over the device. That progressed with time and was fully bridged at 26 weeks. Traditional pedicle screws and autograft in the same model do not achieve the same biological response.
Feedback from local spine surgeons has been positive thus far, Walsh says. “The more they see and understand what we were thinking, the more applications they see for it.”
Thru-Fuze has completed preclinical testing and has been submitted for worldwide patent protection. Walsh and Pelletier are now considering their regulatory strategy.
The plan is to conduct the first clinical trial in Australia with a small cohort of patients, made possible by The New South Wales Medical Device Fund, which provided AU $1.59 million to this effort.
Walsh credits teamwork and collaboration with multiple groups from industry, investors and the research community for the creation of Thru-Fuze: Orchid on development; insights from Andy Carter, an orthopaedic and spine industry executive; Xinova for handling the intellectual property; the facilities and resources available to them at UNSW and their funders.
Because of this, Walsh says, “We feel like we have covered the components of a successful development.”
Images Courtesy of The University of New South Wales