Adaptive designs have emerged as an attractive alternative to traditional clinical studies due to the potential to reduce resources, time and costs. While the structure of these trials offers manufacturers clinical and business benefits, several critical components must be considered to determine whether such a trial design fits your product’s and company’s needs.
In May, FDA released a draft guidance on the principles and benefits of adaptive designs, bringing the concept to the forefront. One of the defining features of adaptive design is flexibility during data collection. Companies are able to learn from the results of the study during its course. Preplanned study changes, such as interim analyses and goals, are set before the study begins. If goals are met by that analysis point, companies can stop enrolling patients and submit their data to FDA.
This differs from traditional or fixed studies, for which factors must be specified at the start of the study and remain unchanged.
“FDA’s guidance clarified that adaptive design is well understood within the Agency and therefore, if it’s applicable to your clinical program, it can help you collect data, have the data submitted to FDA and move forward with your commercialization plans in a more efficient manner,” says Vicki Anastasi, Global Head of Medical Device & Diagnostics Research at ICON. “You save patients, money and time to market. For FDA, that is important. If you can enroll 100 patients vs. 300, that benefits everybody. What we’re seeing from executive teams of companies is that people are looking at adaptive design as a good business model. Having more data and the ability to have data to then make decisions always tends to be a good business model.”
Adaptive design studies can be used throughout the clinical development of a device, from feasibility studies to pivotal clinical trials. Companies can consider an adaptive design for Premarket Approval applications, 510(k) submissions and Investigational Device Exemption. However, the study must be pre-approved by FDA. Thus, it is necessary to allot enough time to coordinate protocol and design with FDA and external experts.
“It could take longer to negotiate the validity of the plan with FDA,” says Kevin Liang, Ph.D., Managing Director at MileStone Research. “There should always be a good level of collaboration with FDA, but adaptive designs are more complicated, so there’s probably more FDA interaction, upfront discussion and negotiation—which is really just time.”
Pre-planning is one of the major differences between adaptive designs and traditional designs for clinical studies. The adaption must be described in the protocol and Statistical Analysis Plan submitted to FDA. Submissions should also detail key issues related to study monitoring and the role of the data monitoring committee, as well as the study decision points to document evidence of safety and effectiveness.
“You have to do a lot more strategic planning on why you’re doing it and how you’re going to do it,” Liang says. “Then, you have to do statistical planning on what these models look like. You have to predict what’s going to happen and then when that happens, you can make a decision to go a direction that you have already defined. It’s like looking down the road and saying, ‘If we get over here and hit this checkpoint, then we can either go left or right. When we go left, then we have to take six steps.’ You have to define that up front, rather than make a decision when you get to that point.”
Having the ability to access the data produced by a study at certain intervals can allow companies to hit their defined goals earlier, or see that they aren’t hitting those marks and change course.
“Your goal may be to have flexibility on the number of patients enrolled because you have only estimated what the results will be,” says Kevin B. McGowan, Ph.D., Director, Regulatory Affair at Musculoskeletal Clinical Regulatory Advisers. “An adaptive design can allow you to make pre-planned assessments during enrollment and enroll additional patients if needed.”
What is the Best Use of Adaptive Design?
FDA’s recent draft guidance highlighted advantages of several prospectively planned adaptive study designs.
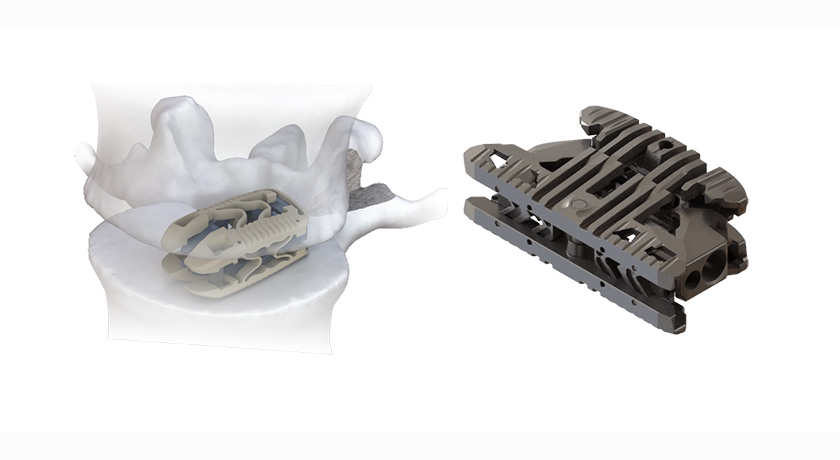
Example: A sponsor conducted a randomized trial of a novel bone graft device designed to demonstrate non-inferiority to an autologous bone graft. An optional, prospectively planned, interim analysis to assess aggregate fusion outcomes (blinded/masked by treatment group) was included in the study design to permit adjustment of the sample size, if necessary.
Example: A randomized non-inferiority study compared an artificial cervical disc to the standard of care of anterior cervical discectomy and fusion. Although the study was sized for 500 patients, a planned interim look when subject number 340 reached the 24-month follow up, demonstrated success. The PMA was submitted to FDA and approved based upon this smaller data set. This is referred to as “group sequential design” and, in many instances, has led to shorter and smaller trials.
This is important in orthopaedic and spine device clinical trials that often have lengthy enrollment periods and follow-up durations of two or more years.
“When you’re conducting a study and you have interim analysis and see that you’ve hit your efficacy goal endpoint early, you are actually then allowed to stop enrolling,” Anastasi says. “You still have to continue to follow up with enrolled patients, but you can go to the panel or FDA much earlier because you met your endpoint. Conversely, it’s also of tremendous value if you get to that interim analysis, look at your endpoint and realize that it’s underpowered and you’re not going to hit it. You can end early for futility or decide to repower your study. If it’s that much underpowered, clients usually end early for futility, take the cost savings for ending the study early, then redesign the product and start a new study.”
Adaptive designs work better for longer term studies with variable enrollment and a longer follow up, as they benefit from ample time and data to pre-determine changes.
“Adaptive studies are generally not useful in studies that have a shorter follow-up or that enroll quickly, as there is not enough time to review data and make the pre-specified decisions,” McGowan says. “For example, in orthopaedics, studies for hyaluronic acid treatments for pain would not be good candidates for an adaptive design due to their generally fast enrollment and short follow-up timing (three to six months).”
Orthobiologics have the potential to benefit from adaptive designs, as well as more novel devices with fewer predicates to go off of, Liang says.
These design structures are also helpful when a device has a non-inferiority claim.
“If you’re pursuing a PMA and looking at non-inferiority, you want to look at superiority as well,” Anastasi says. “Traditionally, those have been two distinct studies. Build a protocol that is statistically relevant for non-inferiority, conduct it and go forward with your submissions. Then, at some point in time, initiate a secondary superiority study. The cost of that approach can be big, and the time is long. If you look at a two-stage adaptive design, that means you’re taking two endpoints: one non-inferiority and one superiority, and doing a seamless study; it’s a two-stage adaptive endpoint. You have key interim analysis time points in the study during which you examine your endpoint for non-inferiority. When you’ve reached that, you move toward your superiority claim. The data you’re now collecting is in the same study, so you’re enrolling patients the same way. You don’t stop and create a new patient profile. You take your non-inferiority data, analyze it and go to FDA, then proceed to the market with your non-inferiority claim while you’re already collecting data on your superiority.”
This is valuable for device manufacturers, as it allows them to enter the market and simultaneously work for the next claim on that product and build their profile on the market faster, because they’re already engaging with FDA.
Despite the recent attention and potential for improved efficiencies in clinical trials, concerns remain relating to the adoption of adaptive designs.
“A lot of folks who work in the clinical trials space don’t have experience doing these,” Liang says. “There’s a general lack of global expertise behind doing these vs. traditional trials. Part of the Clinical Research Organization (CRO) business and the reason that CROs have done really well is that they have a defined process and they follow that process. Adaptive designs change that process. In that case, it could be hard to find the right partners to actually do the trial effectively.”
Adaptive designs are also challenged by some for greater chances of bias, due to the ability to see data throughout the trial, as opposed to a traditional study in which the data is unveiled at the end, followed by analysis, according to Liang.
Nonetheless, adaptive designs create a different approach to clinical trials in an environment that has been traditionally rigid and inflexible.
As Liang says, “It’s a great pathway for some, but it’s not for everybody.”
Send comments on this article to Carolyn LaWell.